Hip Arthritis
ARE YOU WORRIED ABOUT PAIN IN YOUR HIP OR GROIN?
Over the years have you noticed that you can’t walk as far as before? Or experience an awareness of discomfort in your groin or hip? That you’re getting less mobile than before, with increasing stiffness and discomfort?
The discomfort might not even just be in your hip. You might even have pain in your groin, side of hip, buttock or the front of your thigh as well.
Maybe it’s been going on a long time, and gradually you find you cannot do as much as you once used to. Perhaps you find it difficult to walk, climb the stairs or lean forward when you’re sitting down. You may even have developed a limp from the discomfort you’ve been getting, or even fallen as you’ve become more unsteady and found it harder to “catch” yourself.
All these symptoms can be caused by problems affecting the hip, and if this sounds like you perhaps the time has come to get some specialist advice.
THE GOOD NEWS IS THAT YOU ARE IN THE RIGHT PLACE
Before any medical problem can be treated, the consultant needs to understand exactly what is causing the symptoms – to make a proper diagnosis. And here at the Manchester Hip and Knee Clinic we are particularly well equipped to do this, because our team of specialist physiotherapists and occupational therapists is led by Winston Kim, FRCS (Orth), an orthopaedic surgeon with many years of experience and expertise in diagnosing and treating all problems affecting the hip and knee.
WHAT CAUSES HIP PAIN?
BUT WHAT COULD BE CAUSING THE PAIN?
The commonest causes of pain in the hip and groin are:
- Arthritis (or conditions that may cause or lead to arthritis or early arthritis of the hip joint)
- Muscle/ligament strain/tears (often due to overuse or sports injuries)
- Labral (soft tissue cartilage) tears
It may be that you already have a good idea what the problem is: you may have already been told that you need something doing, either an injection (many different options out there!), key hole surgery to the hip (hip arthroscopy) or a hip replacement or hip resurfacing, or perhaps you have had a hip replacement in the past and wonder if there’s a problem with it now. It may be that you can look back and recall your symptoms gradually worsening from an injury or fall some months or even years back.
THE HIP JOINT
The hip joint is a “ball and socket” joint and is one of the strongest – if not the strongest – joint in the entire body. It is the ball-and-socket shape that makes the hip so mobile.
THE STRUCTURE OF THE HIP JOINT
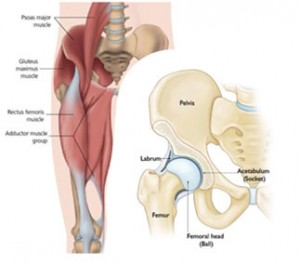
The hip joint is totally surrounded by large, powerful muscles. These muscles add strength and stability to the joint, but it is easy to see how pain from these muscles can mimic pain from the hip joint which lies underneath it. Muscle/ tendon sprains, overuse or overload can cause pain; it is important to differentiate between these and a joint problem.
The on the right side of the image you can see a cut-away drawing of the hip joint itself, clearly showing the “ball-and-socket” nature of the joint.
The head (“ball”) of the femur, the long bone of the thigh, is securely held in the “socket” of the pelvic bone by strong ligaments. The surfaces of the ball and socket joint are covered in very smooth, slippery “articular cartilage” and there is very slippery, lubricating fluid (“synovial fluid”) in the gap between the two bones. This is why in a normal, healthy joint the bones can move easily over each other without rubbing against each other and without pain. The cup is deepened by very strong rings or cartilage called “labrum”. Just like the muscles, these cartilages can become damaged causing pain.
HIP ARTHRITIS
WHAT HAPPENS IN ARTHRITIS OF THE HIP?
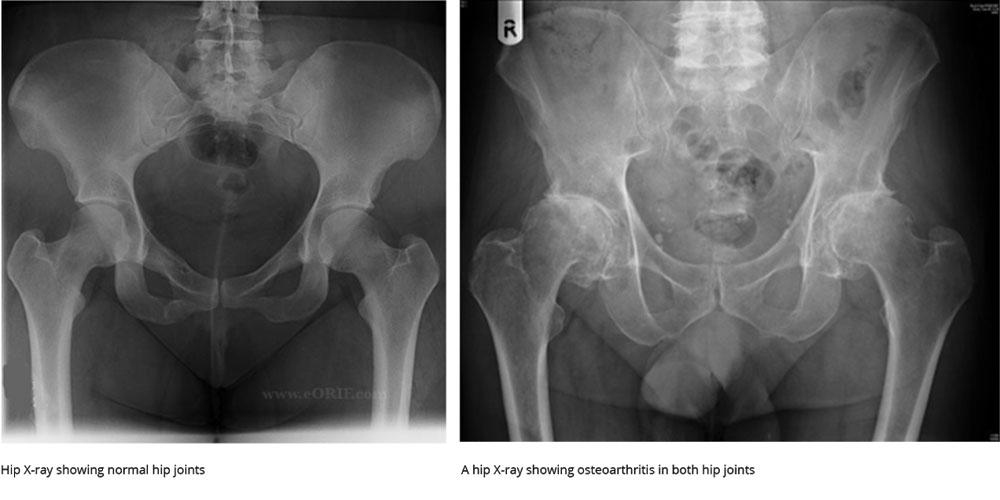
One of the commonest causes of hip pain is arthritis. In arthritis the ‘hard’ cartilage covering the ball and socket gets damaged so instead of gliding freely over each other the bones now grate and rub against each other. This causes further damage to the articular cartilage and later to the bones resulting in aching pain, stiffness and a “creaking” feeling from the joint when you move. Over time this can be very disabling.
IS ARTHRITIS THE ONLY CAUSE OF HIP PAIN?
No. There are small pockets of fluid around the hip called “bursae” and these can become inflamed and cause pain too. This is very common but it is not always clear what has caused it in the first place. It can sometimes be difficult for a doctor who is not an expert in conditions of the hip to distinguish “bursitis” from problems in the hip joint. It is often the case the ‘bursitis’ is due to overuse of the big stabilising muscles of the hip (gluteus medius) and poor healing of a sprain of the gluteus medius. This is known as tendinopathy.
Hernias, muscle and ligament strains (“Gilmore’s groin”) and enlarged glands can also cause pain in the groin, which can be mistaken for pain coming from the hip by the inexperienced. The “labrum” – the rings of ‘soft’ cartilage holding the “ball” of the femur in the “socket” of the pelvic bone can also become worn or torn and this too can cause pain and other problems.
Finally, another common problem is “referred pain”. Because of the way the nerves of the body send information to the brain, the brain sometimes misinterprets where the pain is actually coming from. For this reason, a patient may complain of pain in the hip when the problem causing the pain is actually arising from the back.
This is why it is so important to see an expert in diagnosing and treating problems of the hip and knee, who can accurately diagnose what the underlying problem is and the true source of your symptoms – because unless the cause of the problem is accurately identified it cannot be successfully treated.
WHAT CAUSES OSTEOARTHRITIS OF THE HIP?
We don’t yet fully understand why some people develop osteoarthritis (“wear and tear” arthritis) and others do not. It is certainly linked to previous injuries and childhood hip problems, and worsened by being overweight, although many people develop the condition and often no cause is found. Increasingly, clinical research suggests that Hip Impingement and Hip Labral Tears may predispose some patients to the development of early arthritis.
WHY IS ARTHRITIS OF THE HIP IMPORTANT?
Simply put, because of the inconvenience, discomfort/pain and stiffness it causes. With time, stiffness increases and mobility decreases and this can have a significant impact upon your ability to get around and to live an independent and active life. It can also be really quite painful. Paradoxically some people with very bad osteoarthritis do not have much pain, yet others with only mild osteoarthritis can have very significant pain.
The whole point of treating hip arthritis is to firstly relieve the pain and secondly to increase your mobility, allowing you to live as full and active a life as possible. The good news is that modern surgery – especially joint replacement surgery – is very effective at treating both the pain and stiffness that goes with hip arthritis, and this is one of the real success stories of modern medicine. Keyhole surgery of the hip may also have a role in the treatment of early hip arthritis (‘osteochondral defects’) and cartilage tear (‘labral tears’) of the hip. For patients who have early generalised arthritis, knee injections (see below) may be indicated.
HOW ARE HIP PROBLEMS DIAGNOSED?
First and foremost, the most important thing is that you are seen and assessed by a doctor who is a recognised expert in hip problems. This is because the hip is complex and reaching the correct diagnosis is so important to planning the correct treatment and in achieving the best results for you. There are a number of causes of hip and groin pain, and not all of these are due to a problem in the hip as we have seen. And because it can be difficult to determine where the exact problem lies for a non-specialist, you would be reassured if your symptoms are assessed by a hospital specialist for proper assessment and treatment.
WHAT HAPPENS WHEN I SEE THE CONSULTANT?
Unlike in the NHS where you may be seen by any one of a number of doctors working under the supervision of a consultant, privately you will see a Consultant personally. The first thing I always do is to sit down and listen to you describe exactly what has been troubling you – to take a detailed “history” of your symptoms. I also always ask about any background of injury as well as any other health problems you may have.
After this we will move on to an examination, where I will examine your hip and other joints if appropriate to get to the root cause of your problem.
At this stage I will have a very good idea about the cause of your
symptoms but may need to organise further tests to confirm the diagnosis and to make sure there are no other problems which might be missed. The commonest tests I consider are:
AN X-RAY
An X-ray of the hip is a simple test that gives much information about the bones of the hip joint and is often all that is needed to make a diagnosis.
At this stage I will have a very good idea about the cause of your
symptoms but will need to organise further tests to confirm the diagnosis and to make sure there are no other problems which might be missed. The commonest tests I consider are:
AN MRI SCAN
An MRI (“Magnetic Resonance Imaging”) scan. This is a special scan that does not use X-rays but is especially useful at showing soft tissues and fluid. It is good for looking at the muscles and ligaments around the hip. It is also very useful in picking up a condition called avascular necrosis of the hip, which is commoner in younger people as a cause of their hip pain. It is also used to diagnose early cartilage defects (“osteochondral defects”) and soft tissue cartilage problems (“labral tears”) of the hip.
CT (“COMPUTED TOMOGRAPHY”) SCAN
This is an advanced series of X-rays of the hip which are turned into three- dimensional images by computer. The CT scan is very good at showing “hard” structures such as bone, and is sometimes necessary when planning treatment.
BLOOD TESTS
The commonest problem with the hip joint is osteoarthritis otherwise known as “wear-and-tear” arthritis, but there are other potential problems such as rheumatoid arthritis that can affect the hip too. A blood test is often useful to distinguish between the two problems.
HOW IS OSTEOARTHRITIS OF THE HIP TREATED?
There are several ways of treating osteoarthritis of the hip:
- “Conservative/non-operative management” – in other words painkillers, physiotherapy treatment and exercise
- Hip injections - these include steroid or lubricant type injections (Hyaluronic injections)- see below.
- Surgery
Once I have assessed you and taken any X-rays or scans that might be necessary, I will discuss with you the best way forward. A great deal will depend upon how bad your symptoms are and how much impact they are having on your quality of life, and there is no need to rush into having anything done. My aim is to explain the cause of your symptoms, present the treatment options to you and then to answer your questions thoroughly so between us we can decide on the best treatment for you.
HIP INJECTIONS
Hip injections do not cure structural problems of the hip such as early arthritis of the hip ‘osteochondral defects’, hip labral tears or moderate to severe hip arthritis. However, it may provide improvement in symptoms in patients with mild arthritis whilst you improve your fitness with appropriate exercises and physiotherapy treatment, and allows you time to maximise any benefits from appropriate exercises and non-operative treatment. These injections are performed in clinic, under strict clean techniques (“aseptic environment”).
These injections include:
- Hip Steroid and local anaesthetic injections: This is an anti-inflammatory injection which can improve symptoms by reducing inflammation associated with early to moderate hip symptoms. I’m not a big fan of these injections, but it has a limited role in some patients.
- Hyaluronic Acid injections: These injections aim to improve the viscous and elastic elements of joint fluid, which is affected in patients with hip complaints. Hyaluronic acid is a naturally occurring substance, and unlike steroid injections, may have a cumulative effect in managing symptoms, unlike steroid injections.
- Blood injections. There may be a role for ‘blood injections’ to reduce inflammation, therefore pain, in patients with mild, not severe hip arthritis. Any injection to the hip joint will not cure hip arthritis, but aims to reduce symptoms, in order to provide respite, “buy time”, in order to improve on weight, fitness, muscle strength and general medical condition. The evidence for hip injections is not conclusive, but may be useful for short term, symptomatic relief. Mr Kim and his team will discuss these matters with you in detail during your consultation.
Want to find out more? Speak to one of our team today
Once you have been assessed (by Surgeon, often Physiotherapist), a treatment plan is discussed with you. You will be given time to reflect on the options available to you.
HIP REPLACEMENT SURGERY
A hip replacement is a surgical procedure in which the damaged or worn portions of the hip are removed and replaced with a new, artificial implant made out of a metal alloy stem and ceramic head, and high-grade polymer. Hip replacements are proven, successful operations which improves quality of life for most patients
DO YOU NEED A HIP REPLACEMENT?
You may need a hip replacement if you have difficulties with day to day activities such as walking, climbing stairs or not being able to enjoy your leisure activities as much as you wish due to discomfort or an aching awareness of your hip and stiffness, such as difficulties getting in and out of a car.
A hip replacement is a quality of life procedure which should improve these symptoms significantly. Patients recover well and notice improvement in symptoms and function very quickly after the procedure.
IS HIP REPLACEMENT SURGERY PAINFUL?
You will experience discomfort after a hip replacement but it is usually well controlled by simple painkillers. You will notice a different type of pain compared to the arthritic pain before surgery. These symptoms will improve day by day. The recovery after surgery may take weeks, and it may be 3 to 4 months before you are happy with the procedure. Much depends on your mobility, strength, confidence and fitness before surgery.
POTENTIAL COMPLICATIONS
Although hip replacements are successful operations in the majority of patients, there are risks associated with the procedure you must be aware of and accept prior to surgery. These risks include infection, dislocation (risk of the hip ‘popping out’), leg length difference, clots (‘thrombosis’), stiffness, pain in spite of surgery, incomplete relief of pain after surgery, nerve and vessel damage, re-operation, fracture, medical, anaesthetic and mortality risks. However, you will be reassured we will take every precaution to minimise these risks, including but not limited to, giving you antibiotics before and after surgery, injections or tablets to reduce the risk of clots, surgical stockings and medical care and supervision before and after surgery. Your surgeon will discuss the above as well as reassure you of what is done to reduce risks for you during and after surgery.
INFORMED CONSENT AND CONSENT FORM FOR TOTAL HIP REPLACEMENT SURGERY
THE ANAESTHETIC
You will typically have a regional anaesthetic (spinal anaesthetic), or occasionally for medical reasons a general anaesthetic, and sedation. We will of course, consider your wishes in relation to your preferred anaesthetic. The operation will take between 60 to 90 minutes.
THE PROCEDURE: ‘ROBOT ASSISTED HIP REPLACEMENT’
A curved cut is made, to the side of your hip. Using robotic assisted technology, the hip is excised after taking points around the hip to ensure accurate alignment and size of your new hip. We then fit the implants and trial and test your new hip to make sure they fit and the joint works well and is stable. The advantage of robotic assisted hip replacement is the reassurance that you will have a precisely planned and implanted hip replacement. It would be fitted to your anatomy, size and alignment, which in turn enhances the likelihood of equal leg lengths, a stable hip and a hip that lasts as long as it possibly could last without needing another operation.
Once the new parts are fitted and working the wound will be closed using stitches or staples and covered with a large water-proof dressing, which is kept on for 10 to 14 days after surgery
RECOVERY FOLLOWING HIP REPLACEMENT
You will typically be in hospital between 2 to 3 days after surgery. You will need crutches or a walking aid for several weeks after surgery, depending on your confidence and strength.
Recovery is a balance between rest, taking appropriate precautions in the first few weeks after surgery (to reduce the risk of hip dislocation) and staying active with increasing walks and exercise. A trained physiotherapist and your Surgeon will guide you through your recovery. In general, listen to your hip. If you do too much, your hip will ache. If that happens, you must rest and take simple painkillers, allowing the inflammation and swelling to settle.
ROBOTIC ASSISTED HIP REPLACEMENT
Although hip replacements are generally successful in relieving pain and improving function, patient expectations, higher functional requirements and increasingly younger patients wish a ‘forgotten’/ functionally perfect hip which last their whole lifetimes, whilst enabling them to continue to enjoy an active lifestyle.
Robotic-assisted technology has come about as it is appreciated that the precision and accuracy of hip implant placement can be the difference between a ‘good’ and a ‘forgotten’/excellent hip. In robotic assisted hip replacement surgery, your Surgeon could very precisely (to fractions of a millimetre) implant a hip that is tailored to your anatomy, your hip size and alignment. The outcomes following robotic assisted partial hip replacement are promising, with patients happy that the technical approach to surgery is extremely accurate, so that they are left with just having to concentrate on the rehabilitation required after hip replacement.
Winston Kim, FRCS talks about Mako Hip Replacement
The Alexandra Hospital - Mako Robot - Case Study
CONSIDERING A HIP REPLACEMENT ? : THE NUMBERS OR VOLUME OF HIP REPLACEMENT PERFORMED BY YOUR SURGEON MATTERS
Research has demonstrated that the number of hip and knee replacement procedures performed (e.g. a year) by treating Surgeons matters, * with better outcomes associated with higher volume hip and knee Surgeons.
Mr Kim performed the largest number of private Robot assisted hip and knee replacements in the United Kingdom with more than 1,200 hip and knee replacements performed
According to the National Joint Registry **, Mr Kim performed :
- 489 Hip Replacements (National average approx 124; figures for 2024 TBC)
- 398 Knee replacements (National average approx 120; figures for 2024 TBC)
Outcomes collected in the National Joint Registry reveal very satisfactory clinical outcomes in terms of survivorship of the hip and knee replacements and patient safety over the short and long-term.
In addition to the reassuring data available in the National Joint Registry, patient reported outcomes matter. You will find evidence of several patient reported outcomes by clicking on the various links below.
https://www.iwantgreatcare.org/doctors/mr-winston-kim
https://threebestrated.co.uk/orthopaedic-surgeons-in-manchester
TIPS FOR A SUCCESSFUL OUTCOME
Hip replacements are generally successful operations. However, as it is a technical procedure, it is advisable that your surgery is performed by a Surgeon who has the experience and surgical volume needed to reassure patients of an excellent outcome. Robotic assisted hip replacement may not be indicated for all patients but has the potential to reassure patients in relation to the precision and accuracy of prosthesis implantation.
After surgery, it is important to be patient, to follow surgeon and physiotherapy advice/instructions, to expect that recovery is a process ("good/bad days"), that it may take 4 to 6 months to see significant improvement to your symptoms and function. It is important you understand that compliance with physiotherapy and exercises after hip replacement correlates strongly with an excellent outcome. It is also crucial you understand what may or may not be achievable, that is, your expectations must match what the surgeon and physio believe can be achieved in terms of pain relief and improvement in function from having surgery, taking into account what you were like before surgery.
In short, be patient and rehab well to ensure a good outcome. Mr Kim and his team will ensure that you are seen by trained/specialist physiotherapist and you are fully aware of what is required before and after surgery in terms of patient education, exercises and a fitness and strengthening program of exercises tailored to your needs.
AFTER CARE FOLLOWING SURGERY
The advantages of having your surgery performed privately is that the whole of your care is provided by an experienced Consultant Orthopaedic Surgeon assisted by his team. Your Surgeon will see you daily after your hip replacement, you will have your own room in highly reputable hospitals (BMI the Alexandra or Spire Manchester Hospitals), physiotherapy treatment, medical care will be readily available including High Dependency or Intensive Care facilities if required.
Furthermore, you will have ready access to your Surgeon and his team after discharge from hospital (via a phone call, e mail or outpatient visit, as required).
PRICING (GUIDE PRICE- PLEASE CALL FOR FURTHER DETAILS)
-
- Patient pathway
- Initial consultation
- Diagnostic investigations
- Main treatment
- Post discharge care
- Total
-
- Hospital fees
- N/A
- Included
- Included
- Included
-
- Consultants fees
- £270
- Included
- See total price
- Included
-
- Total
- £15,780 to £17,000 plus
(depending on patient factors,e.g. if High Dependency Care needed, these are fixed price packages provided before surgery, with breakdown and inclusive of follow-ups, full details on enquiry)
TERMS & CONDITIONS
This is a guide price for your consultation and treatment package. Your consultant will be able to discuss treatment options (e.g. conventional v robotic assisted surgery, and whether ITU care required) and costs with you (subject to your pre-assessment tests) so you are able to make an informed decision that's right for you. The fixed cost will be confirmed in writing at time of booking your treatment. Prices can be subject to change.
WAYS TO PAY
There are three ways to pay for your treatment via BMI Alexandra or Spire Hospital.
PAY FOR YOURSELF: Pay for yourself with our fixed price packages. This includes your pre-assessment, treatment, follow-ups and 6 months aftercare
SPREAD THE COST: Pay for yourself with the finance and spread the cost over 12 months, interest-free (terms and conditions apply)
PRIVATE MEDICAL INSURANCE: The cost of your treatment may be covered by private medical insurance (check with your insurer first)
Want to find out more? Speak to one of our team today
Patient Testimonials / Recommendations / Reviews by Patients Treated by Mr Kim and Team
Bernard Sumner, founding member of 2 of the greatest Bands ever (New Order and Joy Division), after successful robot assisted minimally invasive knee surgery, sent 2 overflowing boxes of signed CD’s, vinyl, memorabilia shared by all the team. Surgery by Mr Winston Kim and staff.
Written by a patient
I was diagnosed by Mr Kim in 2014, as having osteoarthritis in my right hip. I was told this was not uncommon as i had been playing football all my life,some of it professionally. Mr Kim was friendly, patient, very professional and explained every aspect of the condition, procedures, choices and possible results of any decisions made. I had suffered with my deteriorating hip for some time and it was now affecting walking freely,at times moving more like somebody a lot older than my 54 years of age. The pain i had at times was intense,mostly in my right groin made worse by the sitting position and especially driving the car,which at times was excruciating. I decided to procede with hip arthroscopy and microfracture, rather than the alternative, a full hip replacement, after considering all avenues, options, and outcomes with Mr Kim. The operation was performed in October 2014 at the Spire hospital Manchester by Mr Kim and i am extremely happy with the results. I am now back in work, moving freely and symptom free, attending the gym 4 to 5 times a week and following Mr Kim’s advice to avoid high impact exercise, like treadmills and to prolong the joint as long as possible. I would highly recommend Mr Kim and the alternative to a full hip replacement even if this means you are just delaying the full replacement to some time in the future. A big thank you again to Mr Kim and everyone at the Spire hospital Manchester who took great care of me.
Written by a carer
The “Go To” Hip & Knee Surgeon…… Winston Kim, to me, is the “go to” Hip and Knee Surgeon in Greater Manchester. I’m a health care professional and have seen him at work. This is a gifted surgeon- the full package- talented, well trained, generous with his time, humble (if that is possible in a surgeon) and above all, a caring Surgeon. I chose to ask Mr Kim to care for uncle Jim at the Alexandra Hospital. I have seen him look after some really tough cases, and many retired doctors and consultants have placed their trust in him, and had him operate on them. My 90 year old uncle had severe longstanding knee pain, but had refused surgery for ages putting up with pain. Mr. Kim picked up the fact that it was referred pain from the hip, even though my uncle had no hip pain. His confidence reassured us. He did a hip replacement, and gave Uncle Jim a new lease of life. “You put your life and your trust in your surgeon’s hands. Mr. Kim has given me back my life and rebuilt my trust….”, reads one of over 100 reviews online on him- check it out for yourself!.
www.iwantgreatcare.org But, I knew that already….. P Ryder, Manchester, on behalf of Uncle Jim, April 2015
Written by a patient
I had a total hip replacement in December 2013 and a total knee replacement 7 days ago. My new hip has given me a new lease of life without pain. I was able to take part in exercise and walking without impingement. I was diagnosed with knee failure in September 2015 and was able to speak to Mr Kim about my knee. He is honest and frank about the exercise in preparation for the operation and rehab. Mr Kim is a caring and highly experienced surgeon. He is supportive to your needs and worries. I hope this is the last operation I will have for a while. I would highly recommend Mr Kim if you want 100% of your life active and pain free!
Written by a patient
I had right hip arthroscopy, carried out by Mr Kim. I was really impressed by the amount of information I received in both the consultation and pre op. The aftercare was superb. After 12 months of continuous pain and discomfort, I had forgotten what normality felt like. 1 week after op felt good, 6 weeks after feel marvellous. A massive Thank you. A.Lewis
Written by a patient
I had a left hip replacement 3 years ago. From the first consultation and throughout the treatment, I found Mr. Kim Most helpful in explaining what would be required for the operation. On the day of the operation he put me completely at ease as this was my first operation & I was very nervous. Post operation he helped me very much and the support staff and physio were excellent in aiding my recovery. I had several reviews to check on the healing & mobility progress all very helpful until I was discharged. I have made an excellent recovery without any disability. Thanks to Mr. Kim
Written by a patient
Male Aged 36 August 2014 – Right hip arthroplasty, labral debridement, microfracture chondroplasty Mr Kim performed a right hip arthoscopy to repair damage in my right hip in August 2014. I had been experiencing moderate discomfort in my right hip for several years, but this had worsened significantly in mid 2013 onwards. I am now 6 months post op and I am pleased to say that the symptoms I was experiencing are beginning to disappear. The rehabilitation process has been quite lengthy – 8 weeks on crutches TTWB post op with a very gradual return to light activity, building up to more progressive exercise from month 4/5 onwards. For the first time in a number of years I feel able to squat and deep flex without feeling a painful ‘clunking’ sensation in my right hip and I am slowly beginning to get back to hill walking and light mountain biking. I am hoping to return to 5 a-side football in summer 2015. For me the key part of the process has been Mr Kim taking time to diagnose my problems and then effectively managing my expectations in terms of the recovery process. He has always taken time to explain the diagnostic and the surgical process and I have always felt entirely comfortable and safe under his care. I would unreservedly recommend Mr Kim. Mike Doyle Cheshire
Written by a patient
I have recently had a replacement hip operation in November 2014 at the Alexandra hospital, the consultant who performed the operation was excellent in his standard of care, before the operation I attended a consultation with Mr Winston Kim, he made me feel very calm and Informed me on the procedure and everything what is involved, everything went really well, also the after care has been excellent, I have felt assured and at ease with the whole procedure , I am so grateful to Mr Winston Kim (consultant) for his care and understanding.
Listen to patients who had Hip Pain, Deciding on Hip Surgery and after Hip Surgery
REFERENCES
- Malik AT, Jain N, Scharschmidt TJ, Li M, Glassman AH, Khan SN. Does Surgeon Volume Affect Outcomes Following Primary Total Hip Arthroplasty? A Systematic Review. J Arthroplasty. 2018 Oct;33(10):3329-3342. doi: 10.1016/j.arth.2018.05.040. Epub 2018 May 31. PMID: 29921502.
- Kugler CM, Goossen K, Rombey T, De Santis KK, Mathes T, Breuing J, Hess S, Burchard R, Pieper D. Hospital volume-outcome relationship in total knee arthroplasty: a systematic review and dose-response meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2022 Aug;30(8):2862-2877. doi: 10.1007/s00167-021-06692-8. Epub 2021 Sep 8. PMID: 34494124; PMCID: PMC9309153. – NJR data from April 2019 to March 2022



